In the past few years, transcatheter aortic valve implantation has been one of the main breakthroughs in the treatment of patients with symptomatic, severe aortic stenosis who are at high risk for surgery. In patients with either self-expandable or balloon-expandable valvular prostheses, transcatheter aortic valve implantation has shown to be technically feasible and has provided an acceptable level of improvement in Hemodynamics as well as acceptable levels of complications; given the characteristics of the patients’ high risk profile, this is all impressive.
Future advances in medical devices may prevent complications caused by vascular injury, stroke, mis-positioning of prostheses, or misplacement causing aortic regurgitation. Although technical issues can cause complications, patient selection is still the main determinant of procedural success.
Selecting candidates for transcatheter valve replacement is a multidisciplinary task that should include cardiologists, cardiovascular surgeons, imaging specialists, and anaesthesiologist’s.
Patient Selection
To determine whether a patient with severe aortic stenosis is a good candidate for transcatheter aortic valve implantation. It is important to consider the person’s symptoms, life expectancy, quality of life, and risk of surgery together with the feasibility of transcatheter aortic valve implantation.
The severity of the disease, evaluation of the aorta and surrounding organs, and assessment of the ilio-femoral arterial system helps to determine who can be treated with transcatheter aortic valve implantation and play an important role in choosing access transfemoral or transapical and which sized valve is best for that patient.
Current imaging modalities, such as echocardiography, multi slice computed tomography (CT), and magnetic resonance imaging (MRI), allow for the assessment of aortic valve morphology, aortic stenosis severity, and anatomy of the aorta and ilio-femoral arterial system, as well as left ventricular dimensions and function.
In this article, we explore how current imaging techniques can be used to evaluate patients with severe aortic stenosis before they undergo transcatheter aortic valve implantation.
Role Of Imagine Technology
Aortic stenosis severity can be best assessed in any of following imaging modalities TTE, TEE, Multislice CT, MRI
Aortic valve morphologies such as Tricuspid or bicuspid can identified by TTE, TEE, Multislice CT, MRI but Valvular calcifications, can be estimated well in Multislice CT, may not be seen in TTE, TEE and cannot be seen in MRI.
Aortic root and ascending aorta
Aortic annulus diameter ,Sinus of Valsalva and Sino tubular junction diameters, Ascending aorta diameter can be best assessed by TTE, TEE, Multislice CT, MRI
Ascending aorta angulation, Coronary Ostia location can be revealed by Multislice CT and MRI
Coronary artery disease can be ruled out by Multislice CT and MRI
Left ventricular dimensions and function, Intra-cavitary thrombus can be estimated in TTE, TEE, Multislice CT, and MRI
Peripheral arteries, Aorta tortuosity and Atheromatosis can be best studied under Multislice CT and MRI
Bulky calcifications and porcelain aorta can be ruled out with the help of Multislice CT
ECHOCARDIOGRAPHY
Echocardiography is the usual non-invasive technique used to diagnose and assess severity of aortic stenosis. Two-dimensional echocardiography can be used to directly visualize aortic valve anatomy (tricuspid/bicuspid) and function. Doppler technology is necessary to accurately determine how severe the stenosis is.
It is critical to evaluate the morphology and severity of aortic stenosis before transcatheter aortic valve implantation. Current recommendations dictate that only patients with symptomatic severe aortic stenosis will be candidates for this procedure. Furthermore, a bicuspid aortic valve may result in a prosthesis mis-deployment, which would cause it to be more elliptical than circular.
Echocardiography enables assessment of left ventricular function and evaluation of concomitant aortic regurgitation or mitral valve disease, thus playing an essential role in evaluation of patients undergoing transcatheter aortic valve implantation.
It is critical to establish the aortic valve anatomy and morphology, including the degree and location of calcifications, prior to transcatheter aortic valve implantation. Bicuspid aortic valve anatomy can be easily detected with trans-thoracic echocardiography.
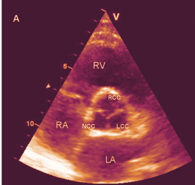
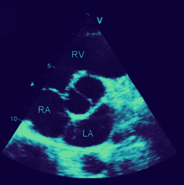
In diastole, from the parasternal short-axis view of a normal tricuspid valve, you should see typical “Y-closure” of the three cusps [Fig. 1(1)] whereas with a bicuspid valve you’ll see two cusps, with two sinuses and a single linear commissure [Fig. 1(2)]. In systole, look for three different sinuses—this will help you define your aortic valve morphology. The evaluation of extent and location of aortic valve calcifications will be covered more extensively in the Multi Slice CT section, it works best as an imaging modality for this purpose.
Aortic Stenosis Severity
The current ACC/AHA recommendations use several hemodynamic measures to determine the severity of aortic stenosis:
- Maximum aortic velocity,
- Mean Trans-valvular pressure gradient
- Continuity equation-derived valve area.
These parameters can be obtained with Doppler echocardiography.
From the continuous wave Doppler recording, maximal velocity can be measured, According to current guidelines, severe aortic stenosis is defined by an AVA of <1 cm2 (<0.6cm2/m2) or a mean aortic valve pressure gradient >40 mmHg,
Aortic Valve Annulus Sizing
There is no established gold-standard method for measuring the aortic valve annulus. The first approach to estimating the aortic valve annulus is transthoracic echocardiography. In the parasternal long-axis view, the diameter of the aortic valve annulus can be measured [Fig. 1:3].
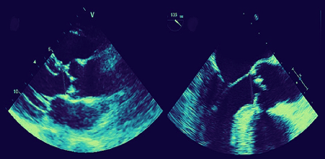
Similarly, transesophageal echocardiography, from a left ventricular long-axis view provides an excellent assessment of the left ventricular outflow tract, aortic valve annulus, and aortic root [Fig. 1:4].
Transcatheter aortic valve implantation is contraindicated when the aortic valve annulus size is < 18 mm or >25 mm for balloon-expandable devices, and 20 mm or >27 mm for self-expandable prostheses, according to current guidelines.
Left Ventricular Dimensions and Function
In patients with severe aortic stenosis, the degree of left ventricular dysfunction is a main determinant in the decision to operate on the valve or not. This is because a depressed ejection fraction (<30%) significantly increases the operative risk but determines a poor prognosis in patients who are not operated on. A less invasive procedure such as transcatheter aortic valve implantation may be an option for those with severe left ventricular dysfunction.
Transthoracic echocardiography is the most widely used examination for assessing left ventricular function. Left ventricular end-diastolic volume and left ventricular end-systolic volume can be measured by Simpson’s rule and the ejection fraction can be derived. This method is especially useful for evaluating left ventricular dimensions and ejection fraction in patients with abnormal left ventricular geometry, a common finding in patients with severe aortic stenosis.
All of these tests can be done non-invasively and quickly with echocardiography. Considering the three-dimensional structure of the aortic valve, however, measurements of the annulus and left ventricular outflow tract size may be vulnerable to geometrical assumptions, resulting in mistakes in disease severity estimation.
The aortic valve annulus is elliptical rather than circular, and the left ventricular outflow tract can be elliptic-shaped as well, especially when sigmoid septal hypertrophy is present. As a result, three-dimensional imaging techniques may be more accurate ways to assess candidates for transcatheter implantation.
Continue Reading : Multi-slice CT, MRI
References: EAE/ASE Recommendations for use of Echo in TAVI: European Journal of Echocardiography, 557-584, Doi 10.1093/jer 086, Text book of TAVI Trips & Tricks

