Intracardiac echocardiography (ICE) is a cutting-edge diagnostic tool that offers an unparalleled view of the heart’s anatomy and function during electrophysiological procedures. This technique allows physicians to visualize the heart from within, providing detailed images of the cardiac structures that are crucial for successful electrophysiology studies.
In this article, we will explore the role of ICE in electrophysiology and delve into the various imaging techniques used to visualize cardiac structure. We will also discuss the benefits of ICE, including its ability to enhance our understanding of the heart’s anatomy and help guide interventional procedures.
Intracardiac echocardiography (ICE) offers dynamic imaging of the vast majority of the heart’s structures in real-time. This allows for constant monitoring of the catheter’s movement and its interaction with the tissue, which enhances the safety and accuracy of catheter manipulations during cardiac ablations.
As new applications for ICE are continually uncovered, the visual library is being constantly updated. Familiarizing yourself with the capabilities of ICE will uncover practical and in-depth views that will streamline your ablations and structural heart procedures.
Transducer location and normal cardiac imaging views
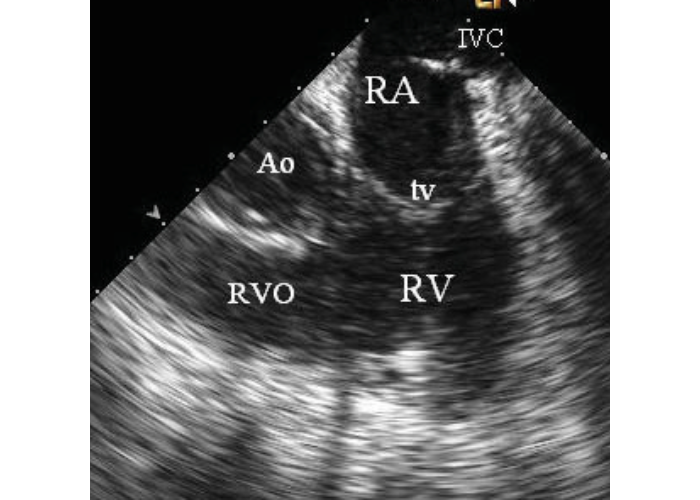
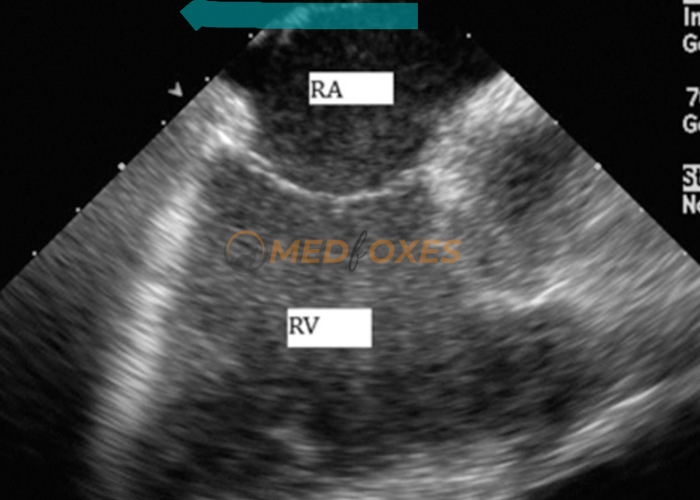
| Catheter position at the IVC orifice, oriented anteriorly and to the left | RA and RV are viewed. (Fig- 1a) |
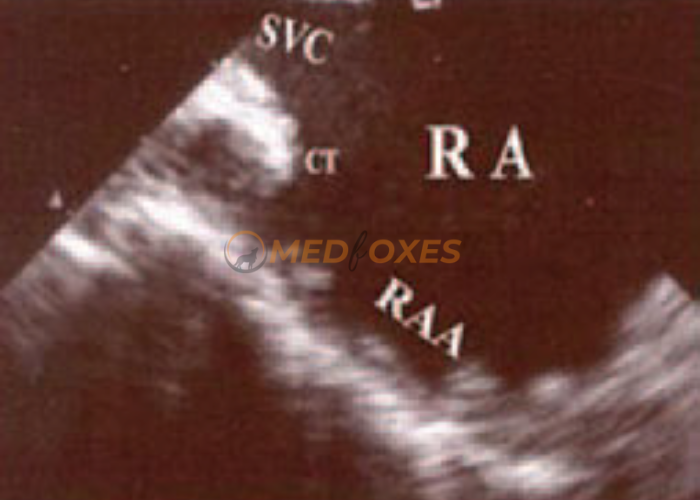
| Catheter position at the IVC orifice With the rotation of the catheter transducer anterolaterally (counterclockwise) | The right atrial appendage is imaged. (Fig- 1b) |
| Catheter position at the junction of the RA and SVC | The superior crista terminalis is viewed. (Fig- 1b) |
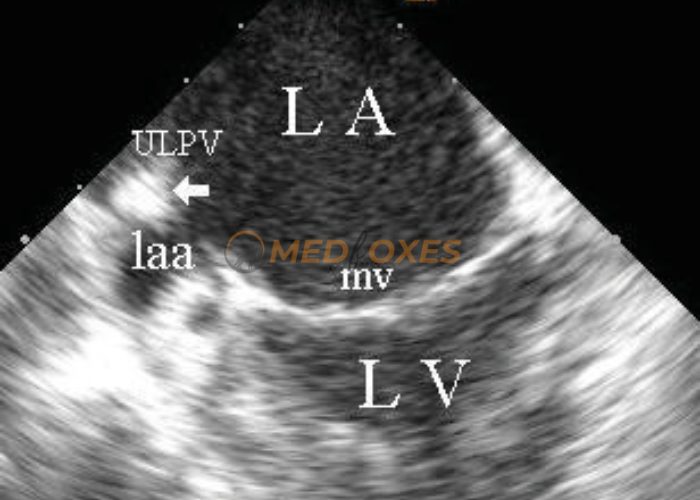
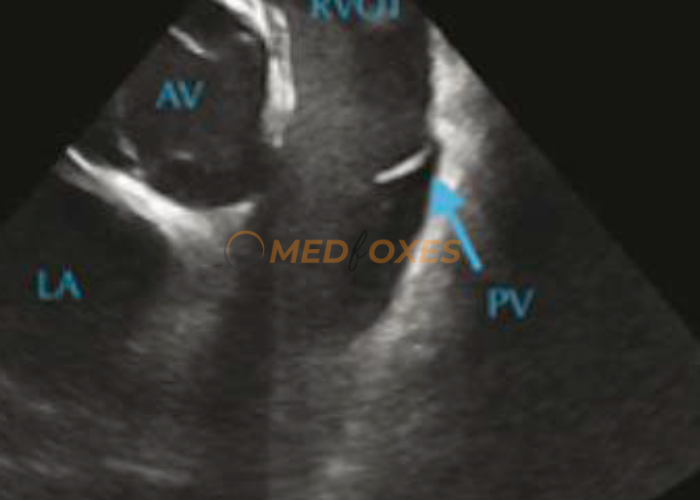
| Catheter transducer placed near the fossa ovalis and IAS, oriented anteriorly and left | LVOT, LAA, truncated LV viewed. (Fig- 1c) |
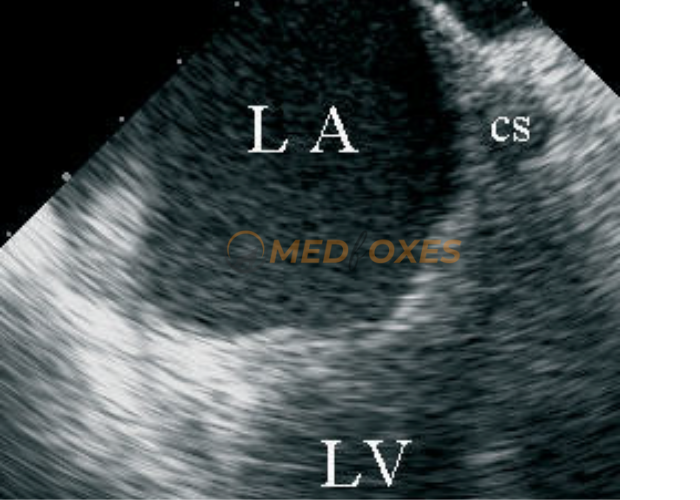
| From above position with CW rotation and slight adjustment of the transducer | LV inflow (MV) and Apex viewed. (Fig- 1d) |
| Continued clockwise rotation of the transducer from above | LUPV and LIPV viewed. (Fig- 1e) |
| From the above position, advance the catheter towards the SVC and rotate posteriorly | RUPV and RIPV viewed. (Fig- 1f) |


Intracardiac anatomic landmarks
There are numerous vital internal heart structures that can serve as reference points during interventional electrophysiology procedures. The techniques for imaging these essential cardiac structures, including normal variations, will be outlined below.
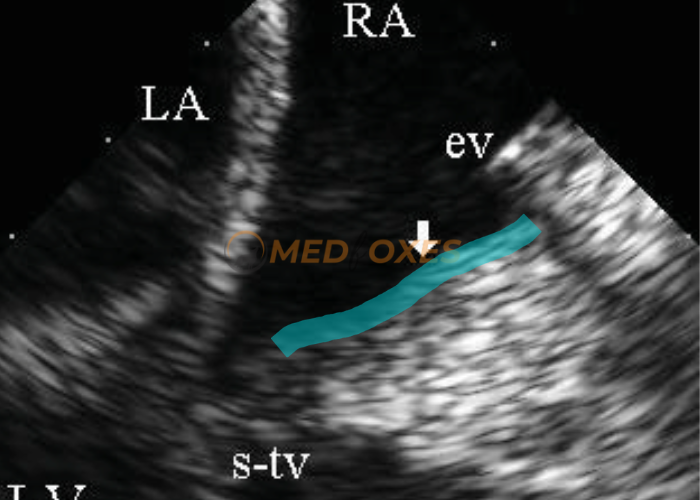
Eustachian valve
The anterior aspect of the opening of the inferior vena cava is surrounded by the eustachian valve. This valve can be seen using intracardiac echocardiography (ICE) when the transducer is positioned in the right atrium close to or above the opening of the inferior vena cava, and it appears as a rim of tissue that is easily visible on the ICE image. (Fig 2.a)

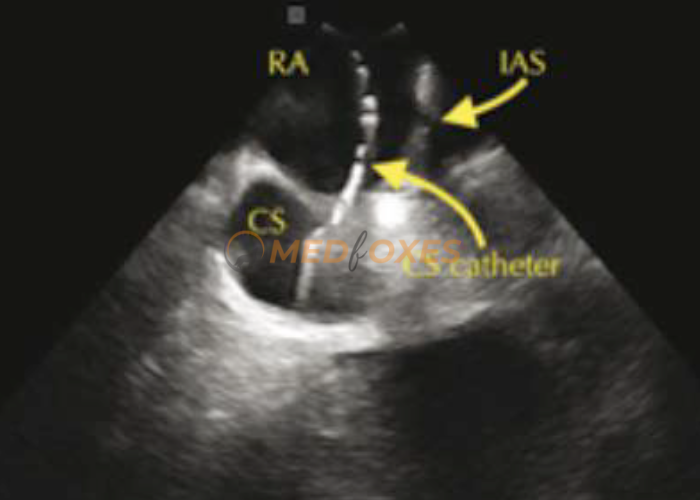
Coronary sinus and its orifice
The coronary sinus is situated along the posterior part of the atrioventricular groove and drains into the right atrium near the inferior vena cava, just in front of the eustachian valve’s central part. The length and width of the coronary sinus, as well as the opening of the coronary sinus, can be seen from the right atrium using the imaging catheter after turning it clockwise from the tricuspid orifice and directing it towards the back of the atrioventricular septal junction and the left atrium. (Fig- 2.b)

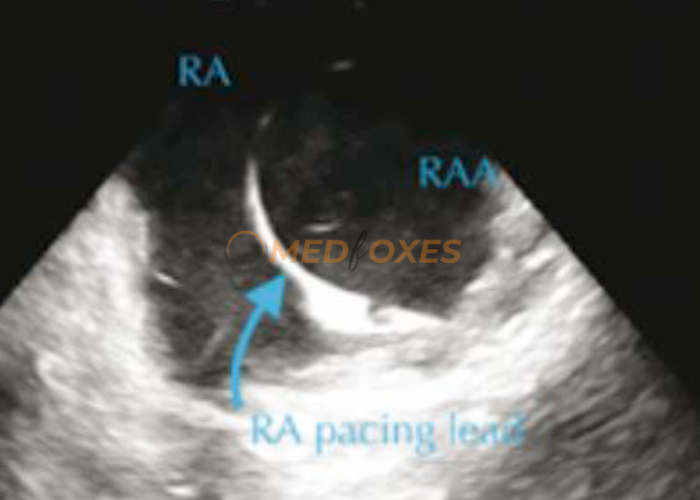
Right atrial appendage
The imaging catheter can be used to view this structure by rotating it counterclockwise from the tricuspid orifice view. Within the right atrial appendage, the pectinate muscles may be visible as a lump. (Fig- 2.c)

Isthmus region
The inferior isthmus and septal isthmus can be seen with the help of an imaging catheter located in the middle or lower part of the right atrium, slightly directed towards the interventricular septum and the point where the tricuspid septal leaflet is attached. It may be necessary to slightly angle the tip of the catheter forward for imaging of the septal isthmus. (Fig- 2d) The isthmus has a muscular wall with a thicker appearance between the orifice of the inferior vena cava and the connection point of the tricuspid valve.
Cardiac Structures
Right Atrium
The Cavo-Tricuspid Isthmus (CTI) can often be seen in the standard ICE home view, which can be further improved by a slight anterior deflection and pulling it back. Utilize both clockwise (posterior/septal) and counterclockwise (anterior/lateral) rotation to thoroughly examine the anatomy of the CTI. This approach allows you to identify the optimal route to navigate around potential obstacles such as ridges, pouches, and crypts and to clearly determine the CTI’s precise boundaries.
The coronary sinus opening (os) can be located by performing a clockwise rotation from the standard ICE home view. The fossa ovalis and the inferior limbus will be in the 1 to 3 o’clock quadrant, with the coronary sinus os located at the 6 o’clock position (Figure 2.e). If the os is adequately sized, the ICE catheter can be used to cannulate the coronary sinus by tilting it forward and maintaining visibility of the os with a gentle clockwise or counterclockwise rotation while slowly advancing the catheter. This technique can provide improved visualisation of the left atrium (LA).
The triangle of Koch can be visualised by performing a slight counterclockwise rotation from the standard home view, which brings the long axis of the atrioventricular (AV) valve into view. The presence of a His catheter can assist in determining the location of this region.
The right atrial appendage (RAA) can be located by performing a counterclockwise rotation from the standard home view while slightly moving the ICE catheter into the 3 to 6 o’clock quadrant. Adjusting the right-left dial to the left can enhance the focus on this area. This technique is useful for the diagnosis of focal atrial tachycardias and monitoring the movement of other catheters in patients with an RA pacing lead. (Figure 2.f).
The crista terminalis can be identified by rotating the ICE catheter counterclockwise from the standard home view, beyond the right atrial appendage, where the pectinate muscles will no longer be visible.
The superior vena cava can be located by performing a clockwise rotation from the standard home view until the fossa ovalis becomes visible, and then tilting the catheter backwards and advancing it. The superior vena cava will be in the 4 to 5 o’clock position.
Right Ventricle
The right ventricle (RV) can be viewed in the standard home view by tilting the ICE catheter forward and using a combination of clockwise and counterclockwise rotation as necessary to bring the desired area into view.
The His bundle area can be located by making a small counterclockwise rotation from the standard home view. This should result in a view of the long axis of the aortic valve and the proximal ascending aorta in the 2 to 3 o’clock position.
The right ventricle view can be obtained by inserting the ICE catheter into the RV by tilting it anteriorly from the home view, using both clockwise and counterclockwise rotation as necessary to keep the opening and closing of the tricuspid valve visible, and advancing it slowly. During this process, the tricuspid valve apparatus will move from the 6 o’clock to the 3 o’clock position. Once the ICE catheter has passed through the tricuspid valve, the dials should be returned to their normal position. (Figure 2.g)
The RVOT can be visualised in the 4 to 6 o’clock position by rotating the ICE catheter clockwise or counterclockwise and adjusting its position slightly forwards or backwards. If necessary, the display can be changed in the ICE console to an up-down orientation, which will show the RVOT at the 10 to 12 o’clock position. (Figure 2.h)
Papillary muscles and moderator band
The transducer can be positioned in the atrium close to the junction of the atria and ventricles or in the right ventricle or right ventricular outflow tract in order to visualize the papillary muscles and moderator band using ICE.
Interatrial Septum
The interatrial septum (IAS) can also be visualised by looking at it from the right ventricle (RV) view. After the RV has been cannulated, a clockwise rotation is applied to move the view through the RV, interventricular septum, left ventricle, and mitral valve until the left atrium (LA) is in sight. The IAS will typically be located between the 8 and 11 o’clock positions. Sometimes, a slight withdrawal is necessary to get a clearer view of the IAS, but this should be done with caution as the catheter can easily be expelled from the RV during this process. Additionally, if present, any pericardial effusions can also be observed in this view. The interatrial septum (IAS) can be viewed by using a clockwise rotation from the home view, along with a posterior tilt if necessary. This will result in a view of the septum. (Figure 2.i)

Using an ICE Catheter to Cross ASD
The interatrial septum (IAS) can be crossed using the intracardiac echocardiography (ICE) catheter in instances where a patent foramen ovale (PFO) or atrial septal defect (ASD) is present. To traverse the defect, the catheter tip should be tilted forward, bringing it towards the defect or wire, and then advanced while keeping the defect or wire in view with slight clockwise or counterclockwise rotation as needed. The IAS and defect or wire will be positioned at the 3 o’clock position. When the IAS is no longer visible, the catheter will have entered the left atrium (LA), offering a clearer view of the LA’s cardiac structures.
Right ventricular outflow tract and pulmonic valve
The pulmonic valve and the infundibulum of the right ventricular outflow tract can be seen by positioning the transducer in the right atrium, facing upwards and towards the front, and then moving it from the right ventricular inlet to the right ventricular outflow.
Left Atrium
The left atrium (LA) can be viewed using an intracardiac echocardiography (ICE) catheter in the right atrium (RA), LA, coronary sinus (CS), and right ventricle (RV). To see the LA when the ICE catheter is in the RA, the septal view should be used. Since the fossa ovalis is thin, the catheter tip should be moved towards the fossa ovalis with a slight anterior tilt.
When the interatrial septum is thick, it often leads to a lower quality image of the left atrium (LA). To orient oneself, the mitral valve (MV) should be located using a counterclockwise rotation. Once the MV is visible, a clockwise rotation should be used to sweep through the structures in a posterior direction. The left atrial appendage (LAA) will be near the MV, in the 4 to 5 o’clock position.
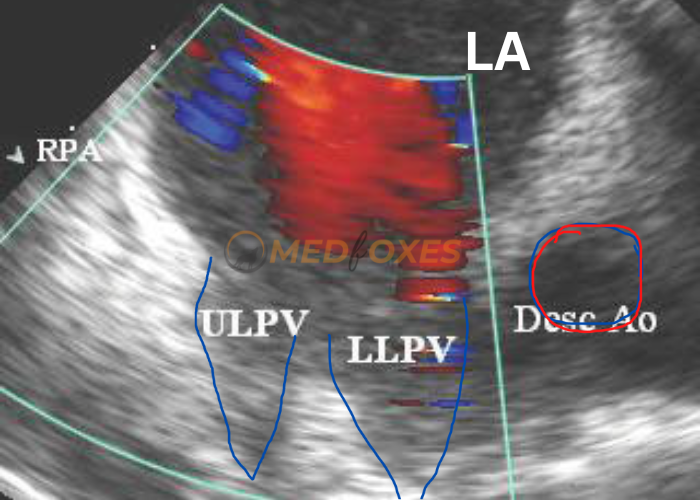
Further clockwise rotation will go through the left pulmonary veins (PV), with the left superior PV appearing first, typically at the 3 to 4 o’clock position, followed by the left inferior PV, which is typically at the 4 to 5 o’clock position. Additional clockwise rotation will sweep through the posterior wall of the LA, where the oesophagus may be seen running horizontally.
By continuing the clockwise rotation, the right pulmonary veins (PVs) will come into view. To get a clearer look at the right PVs, the right-left dial should be turned to the left (Figure 2.j). The right inferior PV will be the first to be seen, followed by the right middle PV if present, and then the right superior PV, sweeping through the 7 to 5 o’clock position. The right superior PV may be easily identified by its proximity to the pulmonary artery.

Ligament of Marshall
The ligament of Marshall can be seen from the right atrium using a transducer with two different cross-sectional views. The first view is a short-axis view that shows the ligament of Marshall between the opening of the left upper pulmonary vein and the left atrial appendage. The second view is a longitudinal cross-sectional view that shows the ligament of Marshall between the distal coronary sinus and the openings of the left pulmonary veins next to the front of the left wall of the descending aorta. On an ultrasound, the ligament of Marshall looks different and is easy to spot because it is more echogenic than the other tissues.
Left Ventricle
The left ventricle (LV) can be best viewed from the right ventricle (RV) view. After accessing the RV, perform a clockwise rotation to move through the RV and interventricular septum and reach the LV. If desired, the image can be reversed from right to left through a change in the console settings, making it similar to a parasternal long-axis view as seen in transthoracic echocardiography.
Identifying the papillary muscles can be difficult as they are both located near the LVOT. Generally, the anterior-lateral papillary muscle will become visible through CW rotation, causing the LV to look shortened. The posterior-medial papillary muscle can be seen through CCW rotation, and the LV will appear more complete.
The mitral valve can be viewed by using the septal view and tilting it anteriorly. By rotating the view counterclockwise, the front part of the valve structure will become visible, while rotating it clockwise will display the back components. When using the RV view, the mitral valve can be examined by rotating the view either clockwise or counterclockwise. The anterior part of the valve is located close to the LVOT, while the posterior component is near the left atrial appendage.
Aortic Valve
To get a clear view of the coronary cusps of the aortic valve, one can use the short-axis view, which can be obtained through the RV view. Once the RV is accessed, rotate the catheter clockwise to go through the RV, the interventricular septum, the LV, and the MV, until the LA becomes visible. If necessary, the catheter may have to be pulled back slightly.
The left coronary cusp should be seen between 4 and 6 o’clock, the right coronary cusp between 12 and 3 o’clock, and the non-coronary cusp between 7 and 11 o’clock. The openings of the right and left coronary arteries can be seen through ICE, aided by colour flow Doppler. (Figure 2.k)

You May also intrested:
Intracardiac Echocardiography Catheters
Non-Fluoroscopy ICE Catheter Manipulation
Intracardiac Echocardiography Catheter Manipulation Technique

