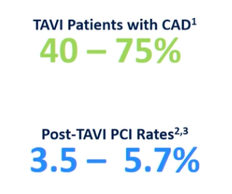
The prevalence of coronary artery disease in patients with severe aortic stenosis undergoing TAVI ranges from 40% to 75%. According to single-center studies, between 3.5% and 5.7% of TAVI patients required PCI after TAVI.
“As the indication for TAVR expands to lower risk patients with a better long-term prognosis, the need for repeat coronary angiography and PCI will increase due to progressive coronary artery disease and the development of acute coronary syndrome.”
Factors Impacting coronary access
Anatomical (Fig-A)
- Sino tubular Junction
- Sinus height
- leaflet length and bulkiness
- Sinus of Valsalva width
- Coronary height
Device and Procedural (Fig-A)
- Commissioner tab orientation
- Ceiling skit height
- Valve implant depth

SYNTAX scoring following TAVI
The linear relationship between Syntax Score and major adverse cardiovascular events (MACE) in patients undergoing TAVR is primarily driven by higher cardiovascular mortality. The number of incomplete revascularization was higher in patients with a higher Syntax Score of >22, and the number of major cardiovascular events was noticeably higher in patients with a residual Syntax Score in the upper tertile of >14. The angiographic appearance or absence of CAD (>70% epicardial artery stenosis and/or>50% left main stenosis) was not associated with adverse outcomes after TAVR. However, when ranked by Syntax Score, patients with a score>33 experienced a higher risk of mortality at both 30 days and 12 months when compared with those with an inter-mediate and low Syntax Score.
Coronary Re-access In Self-Expanding Versus Balloon-Expandable Valves
It is evident that valve design makes a difference in terms of ease of re-access because the self-expanding valve is associated with greater challenges in coronary angiography and PCI post-TAVR. Considering the possibility of coronary re-access in patients with established or intermediate CAD lesions, especially in younger and lower-risk patients, a heart team discussion on the management of CAD in patients with severe AS would be beneficial.
A personalised approach to 1) the treatment of both diseases (e.g., PCI then TAVR vs. Surgery), 2) which coronary lesions to intervene before TAVR, and 3) valve choice, which may affect coronary re-access, is suggested.
Multidetector computed tomography (CT) can be beneficial in determining the anatomy and strategy of coronary re-access. However, there are a variety of practical limitations on utilising this imaging modality in everyday life: 1) When emergency cardiac catheterization or PCI is required, such as in the case of acute coronary syndrome, CT cannot be performed. 2) It can be a logistical challenge to plan a CT before an elective catheterization, especially in terms of the intravenous contrast medium load in patients with renal insufficiency and 3) Motion artefacts and image quality may limit the ability to visualise the transcatheter valve’s leaflet orientation.
relative to the coronary ostia, making it difficult to determine whether the commissural post may impede the ability to re-access coronaries. Nonetheless, it is necessary to understand the 3-dimensional geometric interaction among the valve prosthesis, the aortic root, and coronary ostia to help predict and prepare for challenging issues of coronary re-access in these patients.
The geometric relationship between self-expanding and balloon-expanding valves and coronary ostia
Due to the potentially fatal severity of this uncommon event, acute coronary blockage is the primary focus of pre-procedural preparation. Nevertheless, to date, there has not been any emphasis on factors that will impact future coronary re-access, including valve design and selection, positioning during deployment, as well as potential interactions between the transcatheter valve and the native aortic valve leaflets, coronary ostia height, and sinus of Valsalva diameter and height.
SELF-EXPANDING VALVE: The Core Valve self-expanding valve is composed of 2 parts: the self-expanding nitinol support frame with diamond cell configuration and the tri-leaflet porcine pericardial tissue valve. The frame has 3 levels(Fig-B):
- The high radial expansion force from the inflow aids in stabilising the frame across the annulus.
- The concave middle section allows the frame to avoid contact with the coronary ostia.
- The outflow is the largest part of the frame and rests in the ascending aorta.

The dimensions of the Medtronic Evolut-R and Evolut-PRO are repositionable. When it comes to coronary re-access, there are several crucial factors to take into account. First and foremost, the depth of implantation must be taken into account, especially in patients with low coronary ostia. Due to their design, these self-expanding valves extend beyond the coronary ostia, but the narrow waist and inappropriately large sinuses ensure that the risk of acute coronary obstruction is low. Implantation depth is crucial to maximising eventual coronary re-access, especially if the ostia is less than 10 mm (Fig-C).

The red marks indicate the position of the coronary ostium in relation to the valve frame, and the red line represents the annular plane. The red x’s depict the closest diamonds that can be used to reach the coronary ostium. An ideally placed valve (A) would make coronary access potentially easier than one with a higher implant (B).
The Evolut-skirt PRO’s height is 13 mm, hence it must be implanted at least 4 mm below the annular plane to prevent the skirt from covering the coronary artery. Because the Evolut-R and Evolut-PRO are recapturable when partly deployed, it is possible to position the valve with such accuracy. In this ideal position, it is feasible to engage the coronary artery in a coaxial fashion, assuming the native aortic valve leaflets will not interfere with the path to the coronary ostium (Figure C-A).
If the valve is deployed high (Figure C-B), coronary obstruction will not happen due to the narrow waist of the valve and adequate sinus of Valsalva width. However, in this situation, selective coronary angiography would be challenging.
A straighter catheter with a short tip, such as a Judkins right (JR)4, could be utilised in this situation, including for left main artery cannulation. Furthermore, during TAVR, there is no reliable and consistent way to assess the position of the trans-catheter valve commissures in relation to those of the native aortic valve. This contrasts with surgical aortic valve replacement, where the commissural frame posts are often aligned to the natural commissures. With the repositionable Evolut-R self-expanding valve, the commissure with the paddle (with the letter C on the tab) is introduced facing the anterior part of the ascending aorta. Despite the fact that the delivery system traverses the aorta and crosses the native valve, it is not possible to determine its final position until after the valve has been released.
Theoretically, a commissure can end up being placed directly in front of the coronary ostium. Since there are three commissures and the valve has 15 rows of diamonds, there is a significant chance that this might occur. Even though the circumferential sealing skirt is 13 mm in height (14 mm in the 34-mm Evolut-R), it rises up to 26 mm at the commissural insertion point (Figure D-A). Coaxial contact of the coronary ostia in this situation would be difficult.
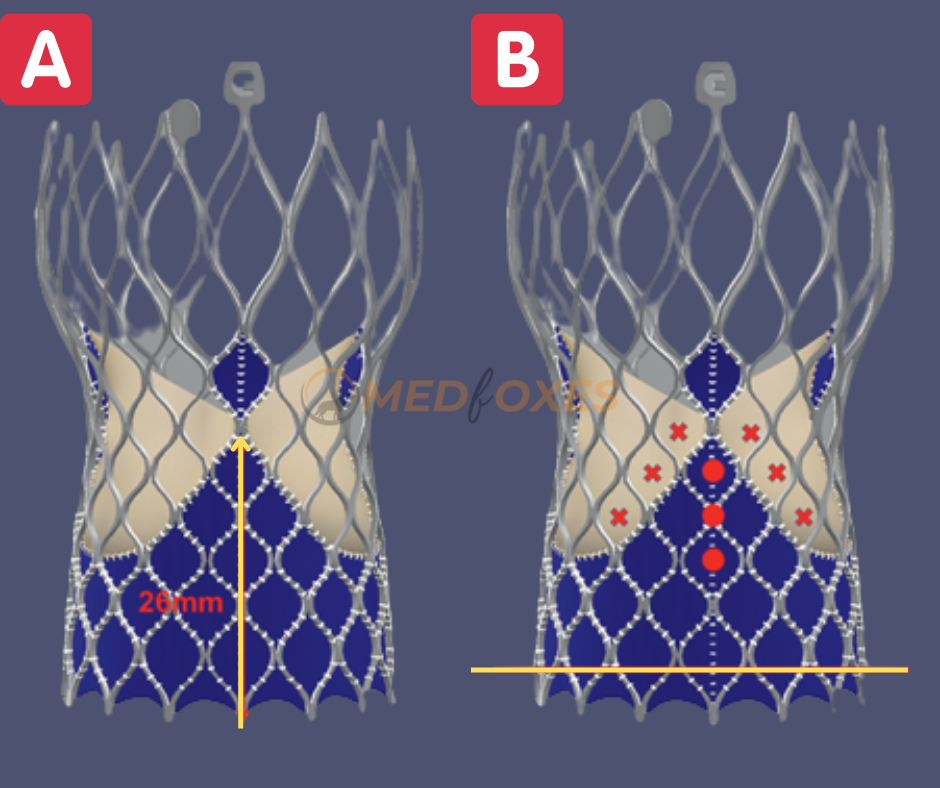
The annular plane is shown by a red line. The three red dots show the heights of the coronary ostia, which are, respectively, 10, 14, and 18 mm above the annular plane. The closest diamonds that can be used to access the coronaries are shown by red x’s. The commissural post of an Evolut-R is 26 mm in height (A). Depending on the height of coronary ostia, a various catheter and approach is essential for coronary re-access, when the ostium faces the side of the commissural post (B).
Scenario
The figure (Figure D-B) demonstrates a theoretical situation where the positionable Evolut-PRO self-expanding valve is positioned 4 mm below the annular plane, consistent with the recommended implantation depth of 3 to 5 mm, and the commissure lines up with the coronary ostia. The three red dots show the heights of the coronary ostia, which are, respectively, 10, 14, and 18 mm above the annular plane. The closest diamonds that can be used to access the coronaries are represented by the cross (X). It is crucial to remember that the width of the sinus of Valsalva defines the distance between the valve frame and the coronary ostia; the broader the sinus, the more space there is to manipulate a catheter toward the coronary ostia, especially in the scenario depicted in Figure D. For non-selective coronary angiography, a narrow sinus would require a fairly acute angle for the catheter to be directed toward the ostia.
If selective engagement is necessary, a guide or a guide extension catheter would need to be inserted into the ostium after a coronary wire has been manipulated into the coronary artery. JL3.5 or JL3, have frequently been used to engage the LCA. On the other hand, a JR4 catheter can typically be used to maintain RCA engagement. The length of the catheter tip would need to be longer if the sinus width was wide because there would be more space between the valve frame and the ostium. JR4.5, JR5, and Amplatz right (AR 2) catheters might be more suited in this situation. CT assessment post-TAVR with the self-expanding valve can assist in identifying potential issues of coronary re-access.
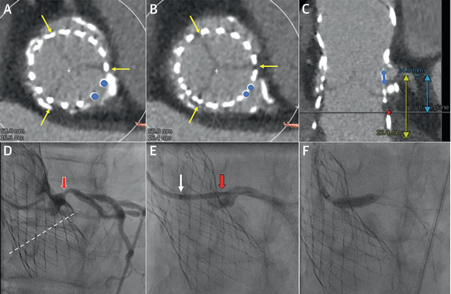
A case of left main PCI post-TAVR with a 29-mm repositionable Evolut-R self-expanding valve is shown in Figure E. The CT evaluation clearly showed that the commissural posts were away from the coronary ostia and the skirt (13 mm) was significantly below the left main coronary artery. As the diamond narrowed towards the centre of the left main artery, coronary engagement was accomplished by trying to come from above, rather than in a coaxial fashion.
Balloon-Expandable Valves
Self-expanding valves have a very different design from balloon-expandable valves. Although it is generally known that acute coronary obstruction is more common with balloon-expandable valves, there is no evidence of serious problems with coronary access following TAVR. This is despite the balloon-expandable valve frames frequently ending up above the coronary ostia. In a CT evaluation of patients post-TAVR with Sapien and Sapien XT valves, partial >1 mm or complete coverage of the left coronary ostium was noticeable in 33.6% and 2.1% of cases, respectively. The right coronary ostium was partially or entirely covered in 42.3% and 7.7% of cases, respectively, whereas in 2.1% of cases, both ostia were totally covered. There were no known problems with patients who later needed PCI or coronary re-access.
The Sino-tubular junction diameter and height is another crucial factor that is essential to the balloon-expandable valves. The balloon-expandable valve frame, particularly Sapien 3, can extend past the Sino Tubular Junction because it does not have a constricted waist like the self-expanding valve, which makes future coronary access from above the valve more difficult or impossible.
Both coronary angiography and PCI can be done in two different ways. First, only a non-selective angiography is likely to be produced if the catheter is inserted slightly above the skirt via the top row of cells. It would then be necessary to use a coronary wire to engage the artery and a railing approach to engage the catheter. Second, a catheter can be utilised to engage the coronary artery from above the Sapien 3 valve if the Sino Tubular Junction is high enough above the valve. From this position, the diameter of the sinus of Valsalva would determine coaxial engagement.
PCI or CAG in TAVI with STEMI.
The femoral approach is suitable in STEMI patients instead of the radial approach. The major use of the femoral approach is aortogram before CAG or PCI. An aortogram is very useful. It will tell you a lot, particularly with the Evolut valve, about the chances of accessing the coronaries. It will often show where the commissures are, so it is easy to know if you have got commissures.
In the Evolut value, there is a C marker on the upper part of the frame and it tells where the commissures are present, so it will also give an idea about whether the commissures of the valve are in front of the coronary ostia or not. It is always recommended to do an aortogram before PCI following TAVI, even if it is the first time or if there have been previous attempts.
Suggested Topics
Multislice CT Imaging on Transcatheter Aortic Valve Implantation
Magnetic Resonance Imaging on TAVI
How Does Imaging Affect Transcatheter Aortic Valve Implantation?