Multislice computed tomography (MultiSlice CT) is the most comprehensive and non-invasive imaging modality to evaluate candidates for transcatheter aortic valve implantation. It can help confirm the severity of aortic stenosis and assess procedural feasibility, as well as device sizing.
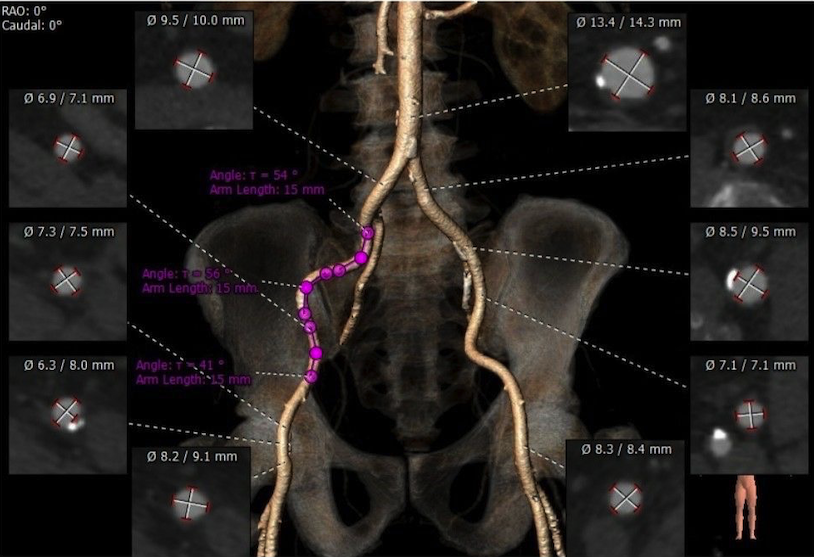
Evaluation of the Peripheral Arteries and Aorta
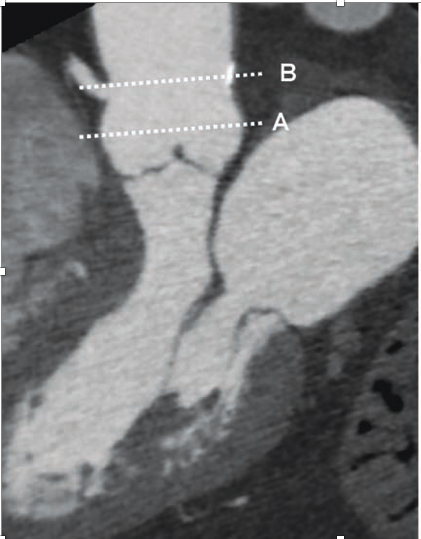
Procedures to implant transcatheter aortic valves, particularly when done via the transfemoral approach, depend greatly on the size, calcification, and branching of the ilio-femoral arteries and abdominal and thoracic aorta. It’s best to get imaging data from pre-procedural angiography, but CT can help determine the diameter of the ilio-femoral arteries.
If arteries have a diameter of less than 6 to 9mm, it is not a good idea to have a transfemoral procedure for this purpose. Bulky calcifications and prominent angulations of the thoracic aorta may necessitate a transapical approach rather than a transfemoral one. Due to the significant risk of vascular problems with the transfemoral route, the transapical approach may be the sole option for performing transcatheter aortic valve implantation in severe aortic stenosis patients with porcelain aorta.
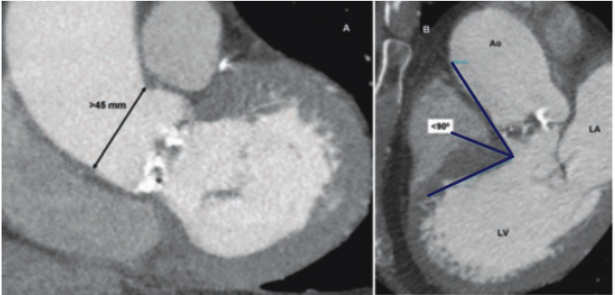
Finally, severe aortic dilatation at the level of the Sino-tubular junction (>45 mm) is regarded a contraindication for self-expandable prosthesis, regardless of vascular access.
Aortic Valve Anatomy and Stenosis Severity
The reconstruction of a coronal and a single oblique sagittal image through the aortic valve after post-processing. (Fig 2:A/2:B) The reconstructed double oblique transverse image at the level of the aortic valve is obtained by aligning both views correctly.(Fig 2:C) The exact anatomy of the aortic valve (tricuspid/bicuspid) as well as the degree and location of calcifications: at the edge of the cusps, the commissures, or the joints of the cusps to the aorta wall may all be determined using this view(Fig 3/4).
Existence of bulky calcifications can be determined from the coronal and sagittal images(Fig 4). As previously stated, these calcifications may cause resistance to prosthesis deployment, resulting in a noncircular deployment, as well as the incidence of occasional but life-threatening problems including coronary ostia blockage. In addition, the area of the aortic valve can be determined using a double oblique transverse image reconstructed at the systolic phase through the points of the cusps.
Aortic valve area may be precisely determined by defining the borders of the cusps during the greatest systolic valve opening, with excellent agreement compared to transesophageal echocardiography or MRI, and strong reproducibility
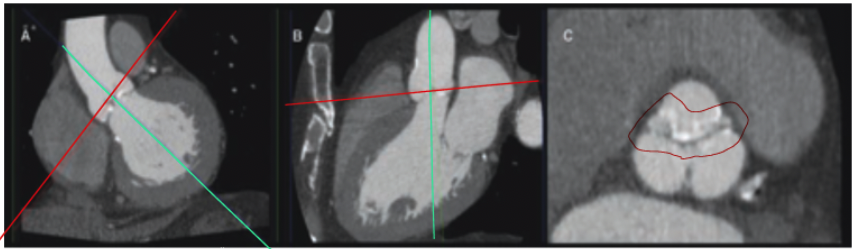

Aortic Annulus Sizing
Accurate measuring of the aortic annulus is one of the most important aspects of a successful transcatheter aortic valve implantation. The aortic annulus appears elliptic-shaped rather than circular in the double oblique views, and the diameter obtained from the coronal view is frequently bigger than the diameter acquired from the sagittal view (Fig. 5 A,B).
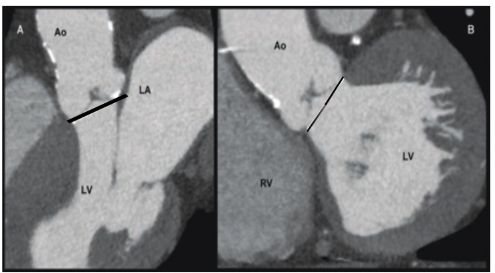
The sagittal view on CT correlates to the parasternal long-axis on transthoracic echocardiography, and both modalities provide equivalent annulus diameters with no significant bias, as previously proven. Two-dimensional echocardiography, on the other hand, cannot estimate the aortic valve annulus diameter recorded in the CT coronal view.
Because the prosthesis size should be as large as feasible, the selection should be made based on the largest diameter of the aortic valve annulus, and transthoracic echocardiography may be less precise than CT in this regard. However, no prospective studies using MSCT measures to determine prosthetic size have been conducted to yet.
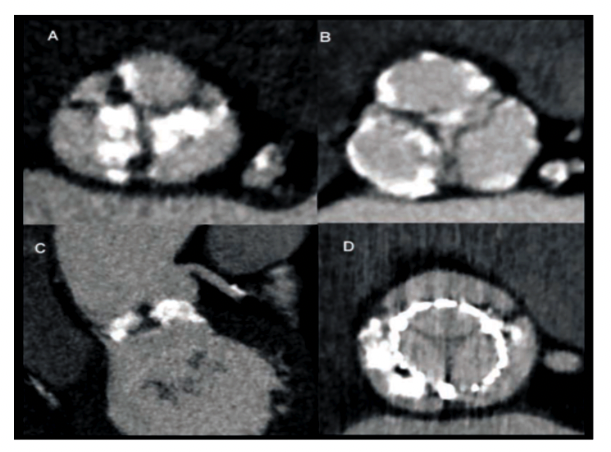
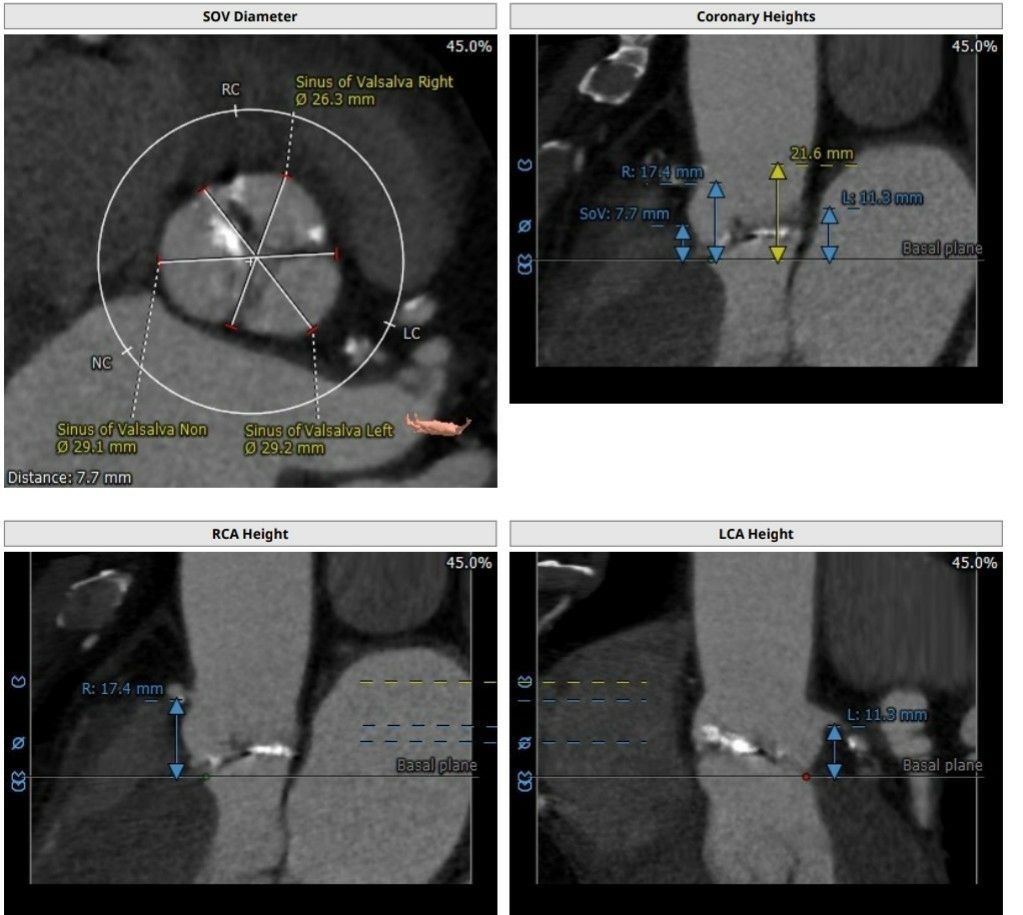
Dimensions of the Aortic Root and Their Relationship to Coronary Arteries
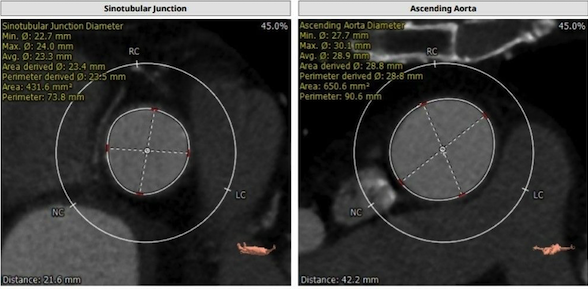
The sagittal and coronal views, as well as the double oblique reconstruction, can be used to determine the size of the sinus of Valsalva. The aortic root’s unique trefoil form at the level of the sinuses may have significant consequences for transcatheter aortic valve implantation (Fig 6).
From the root of the cusp to the contralateral commissure, three distinct sinus sizes can be measured in this image. In addition, the diameter of the sino-tubular junction can be measured in sagittal, coronal, and double oblique views, revealing a circular form.
Sino-tubular junction must be accurately measured before a transcatheter aortic valve can be implanted. A diameter of the sino-tubular junction >45 mm is considered a contraindication, especially for self-expandable prostheses. Finally, the presence of a transverse aorta should be assessed. Aortic root and ascending aorta angulation relative to the left ventricle could indicate transapical implantation of a balloon-expandable device (Fig 7).
Coronary artery examination
Finally, prior to transcatheter aortic valve implantation, a coronary artery examination is required. As previously stated, CT gives precise coronary anatomical data as well as reliable assessment of coronary artery stenosis. Transcatheter aortic valve implantation is not recommended in patients with severe proximal coronary artery stenosis who are not candidates for percutaneous coronary intervention, according to recent consensus statements.
Last but not least, the coronary ostia’s distance from the aortic valve annulus and the length of the aortic cusps should be measured. The aortic valve annulus and the coronary ostia had previously been characterised as having a variable distance, with a mean distance of 14.4 mm for the left coronary ostium and 17.2 mm for the right coronary ostium(Fig 8).
Despite the prosthesis struts that enable blood to pass through, the balloon-expandable prosthesis (Edwards-SAPIEN valve) should be positioned below the level of the coronary ostia. Although the self-expandable prosthesis (CoreValve Revolving System) has a 50-mm height, the device’s unique design, which includes a waist in the middle, renders obstruction of the coronary ostia uncommon.
However, because the sealing annular cuff is positioned in the lower two-thirds of the device, if the distance between the coronary ostium and the aortic valve annulus is smaller, there is still a chance of this procedure-related consequence.
Continue Reading : Echocardiography, MRI On TAVI
References: EAE/ASE Recommendations for use of Echo in TAVI: European Journal of Echocardiography, 557-584, Doi 10.1093/jer 086, Text book of TAVI Trips & Tricks, Computed Tomography Imaging in the Context of Transcatheter Aortic Valve Implantation (TAVI)/Transcatheter Aortic Valve Replacement (TAVR) doi.org/10.1016/j.jcmg.2018.12.003